Substance Use Disorders: Recognizing and Addressing Dual Diagnosis
Substance use disorders often intersect with mental health conditions, creating what professionals call a “dual diagnosis” or “co-occurring disorder.” This intersection can significantly impact a person’s life, making it more challenging to identify correct diagnoses, choose effective treatment options, and achieve long-term recovery. Although these conditions can introduce complexities, understanding the concept of dual diagnosis can help communities, providers, and individuals navigate the path to wellness with greater insight and confidence.
Understanding Dual Diagnosis
Dual diagnosis involves the presence of both a mental health disorder—such as depression, anxiety, bipolar disorder, or post-traumatic stress disorder (PTSD)—and a substance use disorder. Over 21.5 million adults in the United States struggle with co-occurring disorders annually. This highlights how common it is for mental health and substance use issues to overlap. When left unaddressed, these co-occurring conditions can exacerbate one another, resulting in more severe symptoms and a higher risk of complications.
An individual with a severe anxiety disorder, for example, might rely on alcohol or other substances to self-medicate or cope with anxiety symptoms. Over time, that coping strategy can evolve into a substance use disorder. Conversely, a person with a long-standing substance use disorder may develop depression or other mental health challenges as a result of prolonged substance misuse or withdrawal.
The Complexity of Co-Occurring Disorders
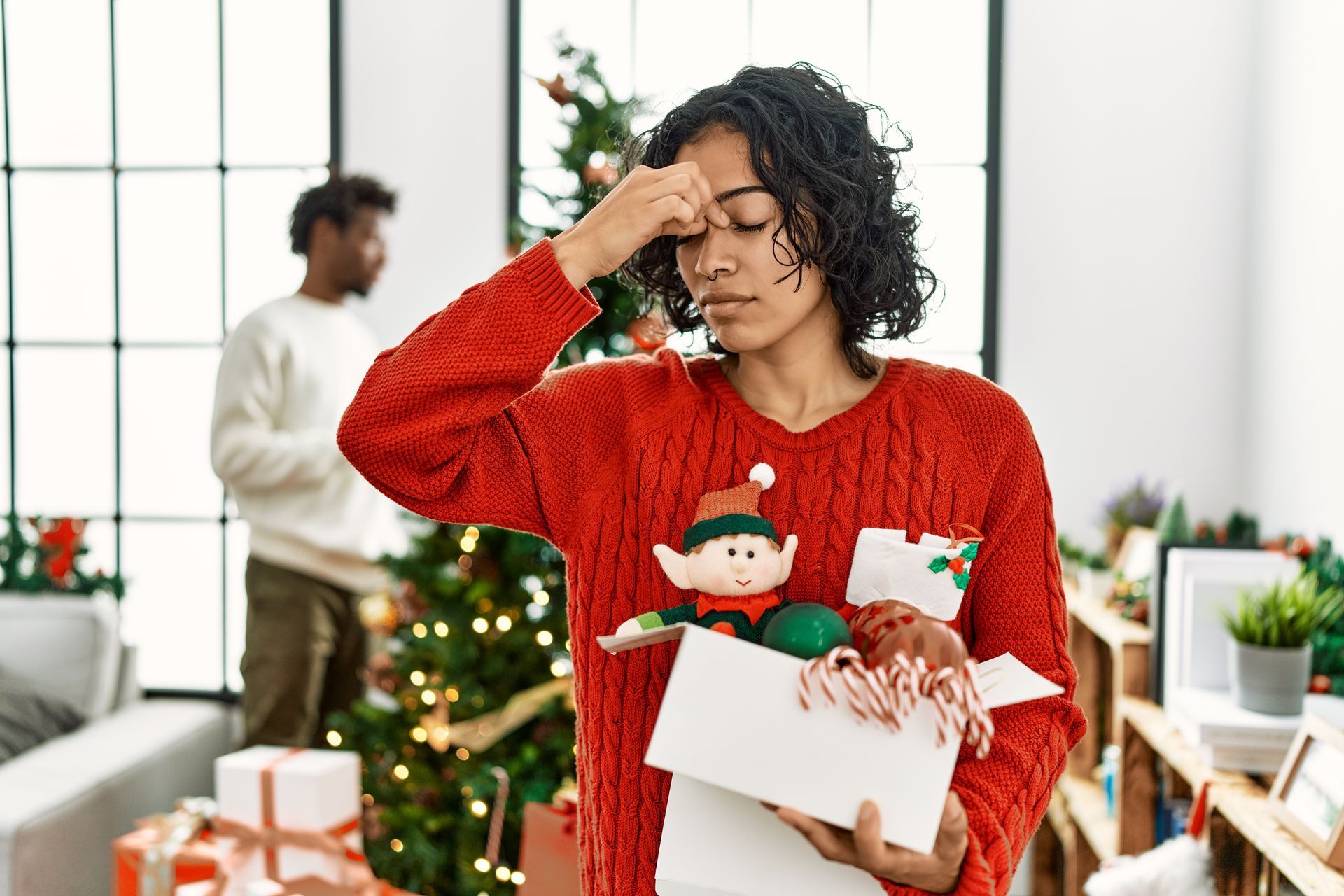
The impact of dual diagnosis often extends beyond the individual’s personal well-being. It might affect interpersonal relationships and employment, and it can strain local healthcare systems. Treating these conditions is inherently more complex, particularly because the symptoms of one disorder may mirror, mask, or even trigger the symptoms of the other.
Stigma can also hinder timely treatment. Individuals with co-occurring disorders sometimes experience shame or feel misunderstood, which can reduce their willingness to seek help. Moreover, healthcare providers may encounter challenges disaggregating the effects of mental health symptoms from those of substance misuse when developing a treatment plan. This underscores the importance of integrated care—a concept where practitioners from different disciplines collaborate to deliver comprehensive support addressing both mental health and substance use.
Integrated Treatment Approaches
An integrated treatment approach recognizes that mental health conditions and substance use disorders operate in a dynamic, interconnected way. Rather than treating each issue in isolation, clinicians look at both holistically. Evidence-based interventions—ranging from cognitive-behavioral therapy (CBT) to motivational interviewing—are often combined with medication management, support groups, and educational programs.
Well-coordinated treatment teams might include psychiatrists, primary care physicians, psychologists, social workers, and other specialized therapists. By unifying expertise under one coordinated approach, there is less fragmentation in care. Patients experience fewer barriers to accessing help, and psychologists or psychiatrists can quickly adjust treatment plans if symptoms evolve. This form of collaboration ensures that medication interactions are managed safely and that psychosocial interventions are adapted to the person’s changing needs.
Medical Community Initiatives in Miami and Austin
Across the United States, many local efforts have emerged to address co-occurring disorders in thoughtful, community-centric ways. Major metropolitan areas like Miami and Austin have taken proactive steps, from public health campaigns to specialized clinics, aiming to reduce the stigma of mental health and substance use issues.
Collaborations between mental health organizations and hospitals have broadened the availability of integrated care programs. Community health centers have worked closely with local nonprofits to improve accessibility, offering low-cost or sliding-scale treatment options for individuals struggling with co-occurring disorders. The city’s emphasis on holistic well-being has led to the growth of programs that promote mindfulness, healthy lifestyle changes, and peer support as part of recovery.
Personalized Care Strategies
Though integrated care serves as a strong foundational approach, successful dual diagnosis treatment ultimately depends on tailoring strategies to each individual’s path. Customized interventions take into account a person’s background, culture, family history, and specific health needs.
Personalized plans may incorporate:
- Changing or adjusting medications to avoid side effects that might exacerbate existing conditions.
- Focusing on specific psychotherapeutic techniques most relevant to the individual’s situation, such as trauma-informed therapy for those who have experienced post-traumatic stress.
- Prioritizing ongoing aftercare support, making it easy for patients to remain connected to resources during and after treatment.
These strategies empower people in ways that a more generic approach might not. When individuals feel valued and understood, they are more likely to remain motivated and engaged in their recovery journey.
Navigating Your Path Forward
Co-occurring mental health and substance use disorders can be daunting, but exploring the range of available treatments helps illuminate a clear, evidence-based pathway. By understanding the nature of dual diagnosis, exploring integrated approaches, and recognizing the importance of personalized care, you can begin taking vital steps toward an improved quality of life.
If you or someone you know is seeking support, Vital Psych MD can help you find a comprehensive treatment program that addresses both mental health and substance use concerns. Our team is dedicated to compassionate, evidence-based care focused on the individual. Contact us today or explore our services to begin your path toward a healthier, more fulfilling future.